 |
| James H. Rimmer, Ph.D., Director |
In addition to the enormously higher rates of obesity observed in people with mental illness, metabolic syndrome is also substantially higher in persons with mental illness compared to the general population. Metabolic syndrome consists of five indicators that increase the risk of heart disease, stroke and type 2 diabetes, and include abdominal obesity (excess body fat around the waist), high triglycerides (blood fats), low HDL (the good type of cholesterol that protects your heart), high blood pressure and glucose intolerance (body can't properly use insulin or blood sugar). In data collected from a large-scale national study, 52% of women and 36% of men with schizophrenia had metabolic syndrome, compared to only 25.1% and 19.7% of women and men in the general population. As shown in the graph, the percentage of obesity and metabolic syndrome in people with mental illness has been reported to be more than two times higher in women and almost twice as high in men compared to the general population.
In a report published in the April issue of the American Journal of Preventive Medicine, the National Institute of Mental Health assembled an expert panel to address the issue of obesity in people with mental illness. The panel focused on two conditions - depression and schizophrenia. One of its major findings was that some of the medications used to control the symptoms associated with mental illness were linked to significant weight gain and metabolic syndrome. However, the expert panel also noted that some of the newer medications had less weight-gaining side effects compared to some of the more traditional, first-generation medications.
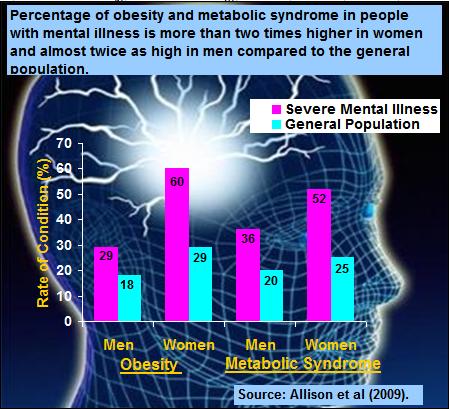 |
| Graph showing the percentage of obesity and metabolic syndrome in people with mental illness is more than two time higher in women and almost twice as high in men compared to the general population |
People with mental illness and their family members should arm themselves with the knowledge and tools needed to prevent or manage obesity and metabolic syndrome. These disorders can, in some cases, cause as much harm to the body and psyche as the condition itself. Keep in mind that some of the newer-generation drugs used to control the symptoms of mental illness may result in less weight gain than some of the older drugs (see American Journal of Preventive Medicine, volume 36, pages 341-350), and that exercise and good nutrition remain the cornerstones of treatment for battling the elements of weight gain and metabolic syndrome. Despite the challenges in motivating many people with mental illness to begin a regimen of proper diet and regular exercise, there are opportunities to encourage healthier lifestyles in this underserved and often misunderstood group. One of the key elements in managing the effects of weight gain in mental illness is adding structure to the day, something that can be achieved with a regular dose of exercise.
Please send any questions or comments to Jim Rimmer, NCHPAD Director at jrimmer@uic.edu.
